Bone Screw and orthopedic plates fixation of fractures has undergone continual design modifications and improvements during recent years. Friedrich Pauwels for the first time defined and applied the tension band principle in nonunions and the fixation of fractures.
This principle of engineering applies to the conversion of tensile forces to compression forces on the convex side of an eccentrically loaded bone. This is done by placing a tension band (bone plate) across the fracture on the tension (or convex) side of the bone. Tensile forces are counteracted by the tension band at this place and converted into compressive forces. If the plate is applied to the compression (or concave) side of the bone, it is possible to bend, fatigue, and fail. Thus, a basic principle of tension band plating is that it must be applied to the tension side of the bone so that the bone itself will receive the compressive forces.
Advantages of Orthopedic Plates
Plates offer the advantages of anatomic reduction of the fracture with open techniques and stability for the early function of muscle-tendon units and joints, but they must be secured from premature weight-bearing.
Disadvantages of Orthopedic Plates
Disadvantages of the plate fixation include stress protection and osteoporosis beneath a plate, the risk of bone refracture after their removal, plate irritation, and in rare cases an immunologic reaction. Plates neutralize deforming forces that can’t be counteracted by only screws. Plates need countering to maintain the optimum stability of the fracture reduction. The application of the screws is also critical. This is because incorrect sequence or placement will result in displacement or shear and loss of reduction.
A researcher named Danis was the first person to design and use a rigid longitudinal compression system. This system results in the healing of fractures without the formation of a visible callus. This kind of conventional rigid plating promotes primary healing through the direct compression of the plate to bone with or without a removable compressor and is now known as the AO/ASIF method (ASIF: Association for the study of internal fixation). These techniques depend on the axial force generated by insertion torque of spherical screw heads to compress plate to bone. It should be noted that not all plating devices depend on this method of compression. In the case of comminuted fractures, lag screws provide the required compression through the purchase of the distal bone fragment.
Although inherently stable, DCPs also have some major disadvantages. These are the damage caused to vascular tissue adjacent to the bone, the bending needed prior to surgical insertion, and most important is stress shielding in the underlying bone. Some researchers advise that necrosis associated with vascular insufficiency, due to the application of bone plates, is the main cause of increased bone porosity. Thus, to decrease the damage of soft tissue, researchers sought the use of plating devices. These devices limit the area of contact between the plate and bone. A variation of the DCP, known as the LC-DCP or locked-compression DCP systems gives stability through locked tapered screw heads while limiting the contact area of the plate-bone. Another method commonly used to reduce stress shielding is to limit the difference between plate and bone rigidities using more flexible plating materials.
Early implants mainly consisted of stainless steel and titanium that can be purchased from Orthopedic Implants Suppliers from India. Interesting to note that there is still much debate between the use of completely rigid systems and systems with increased material flexibility. Some researchers believe that a small volume of micro-motion at the fracture site promotes more rapid fracture healing because a combination of primary and secondary healing can be done in this case. As it is a well-accepted concept, flexural rigidity is dependent both on the material properties and cross-sectional area of the plating device.
In terms of materials, less rigid titanium alloy devices with increased resistance to corrosion have proven to be beneficial and are slowly beginning to replace devices of stainless-steel that previously dominated the market. The experimental evidence discloses an increasing trend towards the general acceptance of more flexible systems, as the level of stress shielding is reduced.
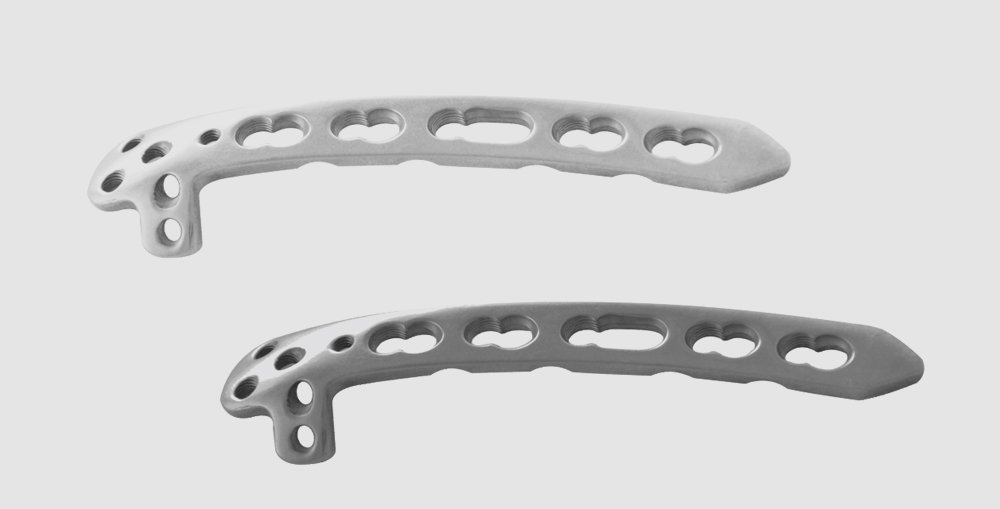
Specific plate designs include tubular plates, spoon plates, T and L plates, dynamic compression plates (DCP), large fragment locking plates, reconstruction plates, distal tibia plate, locking compression plates (LCP), limited contact DCP (LC-LCP).
The many different designs and types of plates can be grouped functionally into three categories:
- Neutralization Plates
- Compression Plates
- Buttress Plates
Neutralization Plates
Neutralization Plates are not a specific type of plate, but neutralization refers to how a plate functions in the fixation of the fracture. A neutralization plate reduces the loading forces on a fracture by spanning the fracture and transferring the loading forces through the plate rather than through the site of the fracture. Neutralization plates are used in conjunction with inter-fragmentary fixation of the screw and neutralize torsional, shear forces, and bending. These are commonly used in a fracture with wedge-type or butterfly fragment after interfragmentary screw fixation of the fracture’s wedge portion. The plate’s stability is significantly improved by the interfragmentary screw. Common fractures fixed with neutralization plates are wedge fractures of the radius, ulna, humerus, and fibula.
Compression Plates
Compression Plates are indicated to apply compression to fractures. The standard compression plate is generally referred to as a dynamic compression plate (DCP), which is a misnomer since these plates provide static compression to a fracture. The holes in the plate have sloped edges on the side of the hole distal from the fracture.
A screw can be inserted in the hole at the end that is close to the fracture. This will lock the plate to the bone without moving the bone in relation to the plate. This is how the screw on the right of the plate was inserted. The screws on the left side of the plate are inserted at the far end of the hole with the screw’s shank touching the far end of the hole. As the screw is inserted, the head will be forced to the right by the slope in the hole, moving the bone and its attached screw towards the fracture compressing.
Buttress Plates
Buttress Plates are employed to rigidly hold in place fractures at the end of long bones, especially at the ankle and knee, where the fracture site experiences large compressive and other types of forces. In order to provide suitable fixation, these plates are broadened and carefully contoured at the joint end of the plate. That is why the buttress plates are referred to as peri-articular plates. The periarticular surfaces of a long bone are complex with several surfaces at each joint. Buttress plates are contoured to a surface (lateral, medial, anterior, etc.), and so many plate designs may be needed for an individual peri-articular region.
There are many buttress plates, and some of the more common configurations are L-shaped, T-shaped, and bulbous end shaped plates. The contoured, periarticular portion of the plate provides a three-dimensional configuration to these plates. Compression plates negate bending, torsional, shear forces and create compression across the site of fracture either through specially designed self-compression holes in the design of dynamic compression plate (DCP). These holes exert compression through the plate’s translation as the screw engages it.