Distal Femur is the part of thighbone above Knee joint, which pans out like an inverted funnel. A fracture in this bone is termed a Distal Femur Fracture.
Such fractures commonly occur in people whose bones are weak due to old age, or in younger people who have suffered high energy injuries like a car crash. In both, the elderly and the young, the injury may extend into the knee joint and may shatter the bone into many pieces.
Anatomy of the Knee
The largest weight-bearing joint in the body is the Knee. While the distal femur bone makes up the top part of the knee, the upper part of the Tibia bone supports the bottom part of the knee joint. The Knee Joint is supported by strong muscles. The muscle in the front of our thigh is called the Quadriceps, while the one at the back of the thigh is the Hamstrings. Apart from supporting, they also allow us to bend and straighten our knees.
Articular cartilage, a smooth, slippery substance covers the ends of the femur. When we bend or straighten our knee, this cartilage protects and cushions the bone.
What is a Distal Femur?
The distal femur is the lower part of the thigh bone (femur), located just above the knee joint. It consists of two rounded ends called condyles, which articulate with the tibia (shinbone) and the patella (kneecap) to form the knee joint. This region plays a crucial role in weight-bearing, movement, and joint stability. It is covered in cartilage to allow smooth motion. The distal femur is often involved in fractures, especially in trauma or osteoporosis cases, and may require surgical intervention. Understanding its structure is essential in orthopedics and sports medicine for diagnosing and treating knee-related injuries and conditions.
What Are the Different Types of Distal Femur Fractures?
There are different types of Distal Femur Fractures. The bone may break in transverse plane or into many pieces (comminuted fracture). Sometimes the fracture may extend into the knee joint and separate the surface of the bone into a few (or many) parts. Such fractures are called intra-articular. Due to damage to the cartilage surface of the bone, intra-articular fractures can be more difficult to treat.
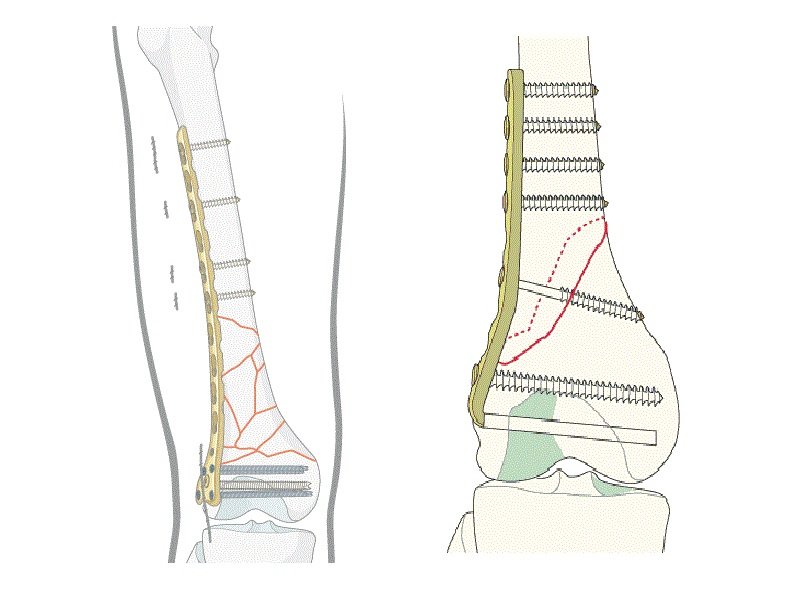
Various fracture types of distal femur:
(Left) A transverse fracture across the distal femur.
(Center) An intra-articular fracture that extends into the knee joint.
(Right) A comminuted fracture that extends into the knee joint and upwards into the femoral shaft.
Distal femur fractures can be closed, if the skin is intact, or can be open. An open fracture is when a bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the broken bone.
Open fractures often have associated damage to the surrounding muscles, tendons, and ligaments. Thus, they have a higher risk of complications and take a longer time to heal.
The hamstrings and quadriceps muscles both tend to contract and shorten when the distal femur breaks. In such a case, the bone fragments change position, and it is difficult to line up with a cast.
Distal femur fracture in which the bones are out of alignment
In this x-ray of the knee taken from the side, the muscles at the front and back of the thigh have shortened and pulled the broken pieces of bone out of alignment.
What Are the Causes of Distal Femur Fractures of the Knee?
As discussed earlier, Fractures of the distal femur occur mostly in younger people (under age 50) or the elderly.
Younger patients suffer high-energy injuries usually caused by falls from significant heights or motor vehicle collisions. Due to the high energy impact, many patients also often have injuries of the head, chest, abdomen, pelvis, spine, and other limbs.
In Elderly people, with age, the bone quality becomes poor. Bones become thinner and become fragile. A lower-force impact, like a fall from standing, can also cause a distal femur fracture. Although elderly patients do not often have other injuries, they may have concerning medical problems, such as conditions of the heart, lungs, and kidneys, and diabetes.
What Are the Symptoms of Distal Femur Fractures?
The most common symptoms of distal femur fracture include:
Pain with weight-bearing
Swelling and bruising
Tenderness to touch
Deformity, the knee may look “out of place,” and the leg may appear shorter and crooked
While in the majority of cases, these symptoms occur around the knee, there may also be symptoms in the thigh area.
How to Treat Femur Fractures?
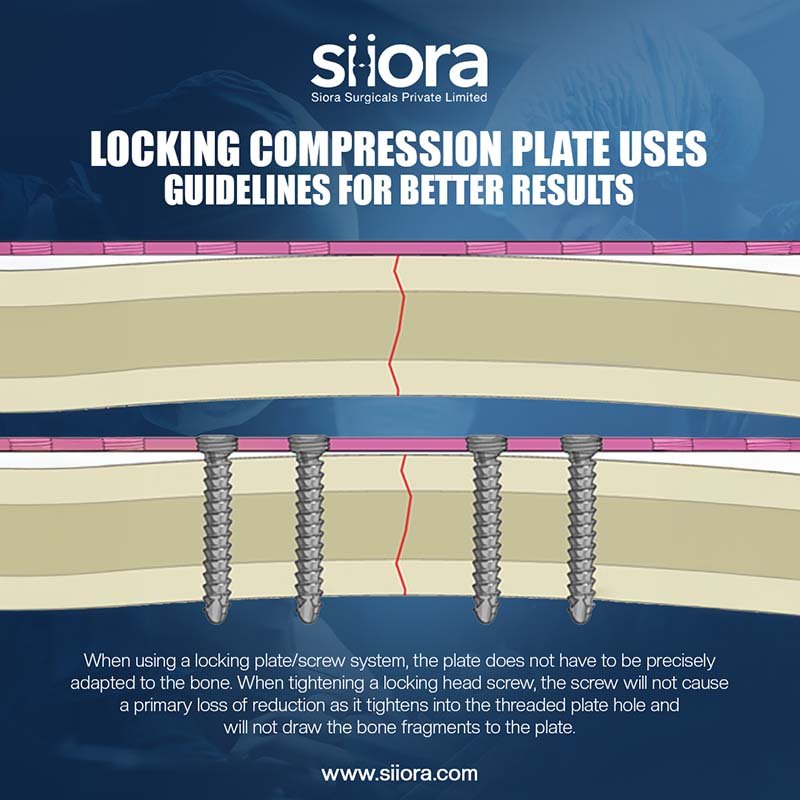
Treating femur fractures typically requires medical intervention and depends on the severity and location of the break. First, emergency care focuses on stabilizing the patient, managing pain, and preventing further injury. In most cases, surgery is necessary. Common surgical methods include internal fixation using metal rods, plates, or screws to realign and stabilize the bone. In severe cases, such as with shattered bones or in elderly patients, a partial or total hip replacement may be considered. After surgery, physical therapy is essential to restore mobility, strength, and flexibility. Pain management and antibiotics may be prescribed if there’s an open wound. Recovery can take several weeks to months, during which time patients may use crutches or walkers. Regular follow-ups with X-rays help monitor healing progress. Early and proper treatment is crucial to avoid complications like blood clots, infection, or improper bone healing (malunion or nonunion).
What is the Fractured Femur Recovery Time?
The recovery time for a fractured femur typically ranges from 3 to 6 months, depending on the severity of the fracture, the type of treatment (surgical or non-surgical), and the patient’s overall health. Most femur fractures require surgery, such as internal fixation with rods or plates, followed by a structured rehabilitation program. In the first few weeks, patients may use crutches or a walker to avoid putting weight on the leg. Physical therapy is essential to restore strength, flexibility, and mobility. For younger or otherwise healthy individuals, healing may be quicker, while older adults or those with underlying conditions may take longer. Full recovery—including a return to normal walking and daily activities—can extend beyond six months in complex cases. Regular follow-up with a doctor is important to monitor healing progress and prevent complications such as stiffness or blood clots. Always follow your orthopedic surgeon’s advice closely for the best outcome.