Orthopedic trauma care has made remarkable progress over the past few decades, especially in the realm of internal fixation devices. Among these innovations, the Locking Compression Plate (LCP) has emerged as a game-changer. Designed to provide stable fixation while minimizing soft tissue damage, LCPs are increasingly used in both complex fractures and routine orthopedic procedures.
However, despite their advantages, successful outcomes with locking plates depend heavily on correct application. In this article, we’ll break down the key uses of locking compression plates and share practical guidelines for better surgical results.
What is a Locking Compression Plate (LCP)?
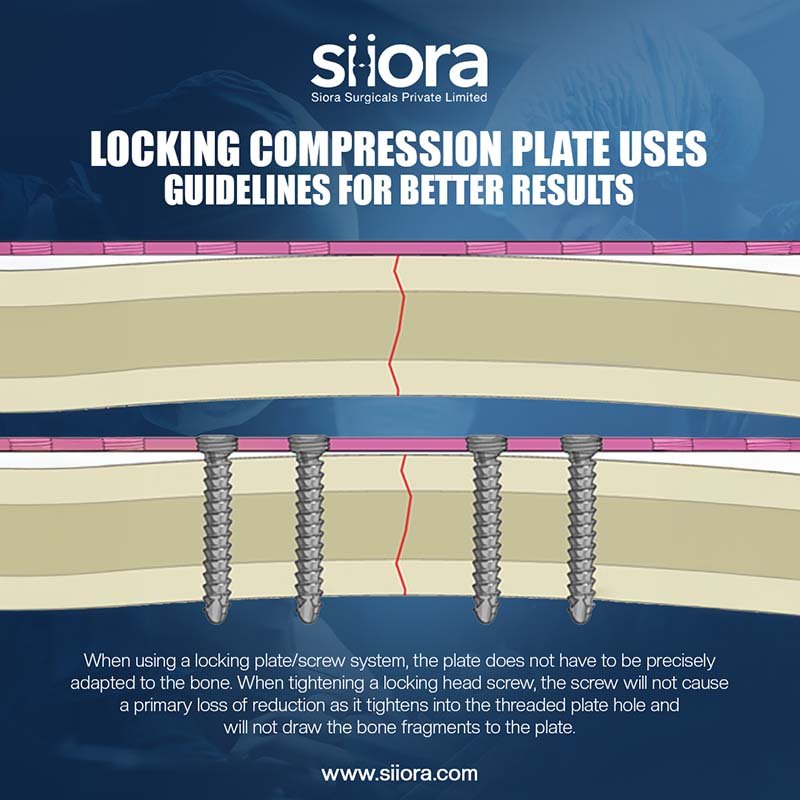
A Locking Compression Plate is a type of orthopedic implant used to stabilize bone fragments. Unlike traditional plates, where the screws press the plate against the bone (creating friction for stability), LCPs use locking screws that thread into the plate itself. This creates a fixed-angle construct that does not rely on plate-to-bone compression for stability.
This difference makes LCPs particularly useful in osteoporotic bones, comminuted fractures, or metaphyseal regions where conventional compression plates may fail.
What Are the Common Locking Compression Plate Uses?
Locking plates have a wide array of applications in trauma and reconstructive orthopedics. Some of the most common indications include:
- Comminuted Fractures
When a bone shatters into multiple fragments, conventional plates may not provide adequate fixation. Locking plates help by forming a rigid frame that maintains alignment without needing each fragment to be compressed directly.
- Osteoporotic Bone Fixation
In elderly patients with poor bone quality, screw purchase can be weak. Locking screws do not rely on bone density for stability, making them ideal for treating fractures in this demographic.
- Periarticular Fractures
Fractures near joints, such as distal femur, proximal tibia, and distal radius fractures, often benefit from LCPs due to their fixed-angle support and minimal disruption to the joint’s alignment.
- Minimally Invasive Plate Osteosynthesis (MIPO)
LCPs allow for biological fixation – preserving periosteal blood supply by minimizing surgical exposure. They can be inserted submuscularly through small incisions, aligning well with MIPO principles.
- Non-unions and Malunions
Surgeons can use locking plates to restabilize and correct alignment in cases where previous fractures haven’t healed properly, without excessively stripping soft tissue.
Guidelines for Better Results with Locking Compression Plates
While locking plates offer advanced fixation, poor technique or inappropriate indications can still lead to complications. Below are practical, experience-backed guidelines to optimize outcomes:
- Understand the Principle – Not Just the Implant
One of the most common mistakes is treating the locking plate as a “fix-all” solution. It’s important to understand when a fracture benefits from locking technology and when a conventional compression plate or intramedullary nail might be more appropriate. Locking plates are not always superior—they’re different and situationally advantageous.
- Choose the Right Length Plate
Always opt for a longer plate than you think is necessary, especially in comminuted fractures. A longer plate helps distribute stress more evenly and reduces the risk of implant failure. As a general rule, maintain at least 3-4 screw holes on either side of the fracture line.
- Follow the Working Length Principle
In bridge plating, intentionally leaving empty holes near the fracture site increases the plate’s working length and improves flexibility. This promotes secondary bone healing through callus formation. Avoid over-rigid constructs, especially in bridging comminuted fractures.
- Mix Locking and Non-Locking Screws Wisely
One of the underrated advantages of the LCP system is its combination of locking and compression slots. Start by inserting non-locking screws to draw the plate closer to the bone (if compression is needed), and then follow with locking screws for angular stability. Rigid all-locking constructs can prevent micromotion, which is essential for callus formation.
- Mind the Soft Tissues
One of the major benefits of locking plates is their compatibility with minimally invasive techniques. Use this to your advantage. Preserve soft tissue and periosteal blood supply whenever possible. Overexposure during open reduction can defeat the purpose of using a biologically friendly implant.
- Avoid Overuse in Simple Fractures
Not every fracture needs a locking plate. In simple, transverse or oblique fractures with good bone quality, a conventional dynamic compression plate (DCP) might be sufficient, and more cost-effective. Use LCPs selectively for their strengths, not out of habit.
- Watch Out for Cold Welding
A practical tip during removal: locking screws can cold weld into the plate, especially if over-tightened. Use torque-limiting screwdrivers where possible, and always clean threads of debris and blood before final tightening.
- Post-Operative Protocols Matter
Even the best fixation can fail if the rehabilitation protocol isn’t followed properly. Educate the patient about partial weight-bearing, especially in osteoporotic or load-bearing bones fixed with locking plates. Too early or aggressive loading can lead to failure.
Final Thoughts
Locking Compression Plates have revolutionized internal fixation, offering a strong and flexible option for treating challenging fractures. But like any tool, their value lies in knowing when and how to use them.
Surgeons must move beyond just understanding the hardware to mastering the biomechanics, biology, and decision-making behind each case. By doing so, we can ensure locking plates fulfill their potential, not just in the operating room, but in the lives of the patients we serve.