Clavicle fractures are very common. They comprise 2.6% to 5% of all fractures in adults, with midshaft injuries accounting for almost 75% of all fracture types. Clavicle fractures typically occur when a the bone experiences an axial load. This is generally in the form of a sudden point load to the apex of the shoulder. When these fractures displace, the proximal fragment is usually pulled superiorly by the sternocleidomastoid muscle. While on the other hand, lateral pulling of the distal fragment is there by the weight of the arm. The management of most minimally displaced clavicular or nondisplaced fractures can be non-surgical by placing the arm in a sling. In these instances, the malunion and nonunion rates are very low.
However, when midshaft clavicular fractures present with complete displacement or significant shortening, the risk of nonunion is significantly higher with conservative management. Surgical decision making is a matter of debate. Currently, the only absolute indications for surgical treatment of clavicular fractures include open fractures and injuries associated with evolving skin compromise. Relative indications for internal fixation and open reduction of midshaft clavicular fractures include injuries with 15 to 20 mm of shortening, fractures with significant comminution, completely displaced fractures, floating shoulder injuries that involve a concomitant glenoid neck fracture, painful non-unions, and midshaft clavicular fractures in some multisystem trauma cases.
Depending on fracture morphology, one can perform either open or closed reduction and intramedullary orthopedic pin fixation or open reduction and bone plate fixation. Orthopedic implants Manufacturers can supply these quality implants. Biochemically, both methods provide similar repair strength for middle-third clavicle fractures. After hardware removal, clavicles previously treated with intramedullary fixation were shown to be stronger. When compared to those treated with bone plate fixation. Clinically, internal fixation and open reduction of clavicular fractures have shown marked success for the union. This too in a relatively expected time frame with low complications.
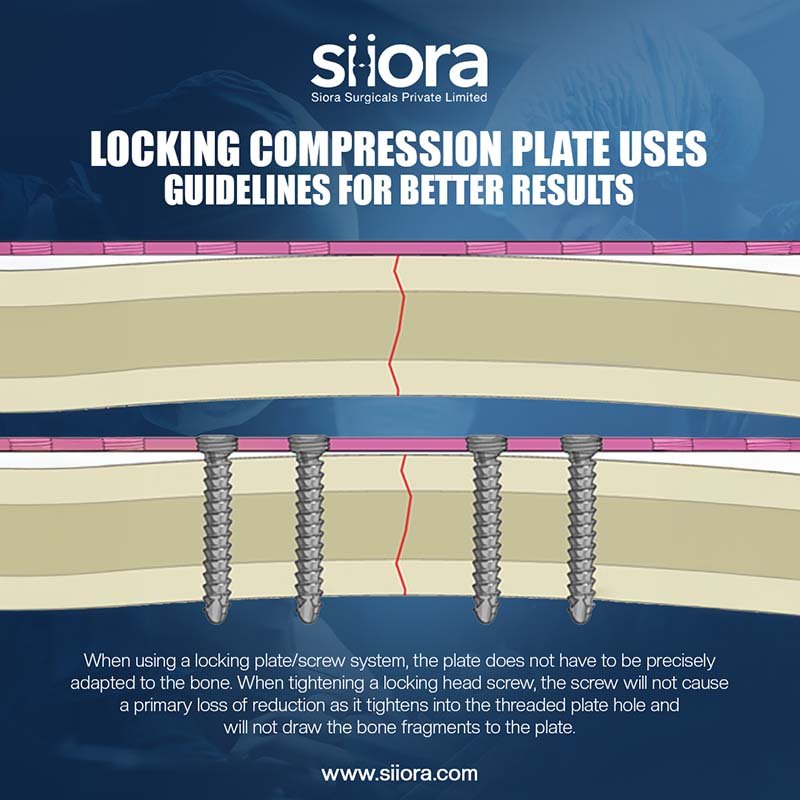
Intramedullary fixation offers the benefit of smaller scars and lower refracture potential. Whereas, it also bears the potential risk of hardware prominence and a little higher incidence of nonunion. General principles for a successful surgical outcome involve minimizing soft tissue disruption and periosteal stripping as much as possible during exposure, achieving an anatomic reduction, and preventing wound complications and hardware irritation as much as possible with suitable soft tissue hardware coverage. One can use either dynamic compression plates (DCP) or locked plating constructs, depending on bone quality and fracture type. In general, the surgeon places orthopedic bone plate on the anteroposterior, or tension side, of the clavicle. This results in the most biochemically sound construct.